Advertisement
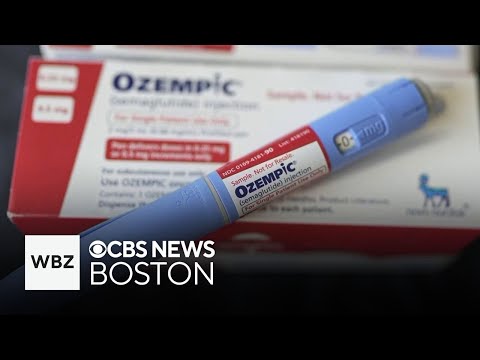
Does Paxlovid really help with COVID-19? The answer is absolutely yes! Recent studies show that taking Paxlovid within the first 5 days of symptoms can reduce hospitalization risk by 80% and cut death rates dramatically. Here's what you need to know: this antiviral isn't just for severe cases - it can help even when your symptoms feel mild. I've been following the research closely, and the numbers don't lie. People who take Paxlovid are 5 times less likely to be hospitalized and 10 times less likely to die from COVID-19 compared to those who don't. That's why doctors are calling it a game-changer in our fight against the pandemic. But here's the catch - timing is everything. You've got to act fast when symptoms appear. Think of it like putting out a small fire before it becomes a blaze. And while it's currently only approved for high-risk individuals in the U.S., new studies suggest expanding access could benefit everyone. Let's dive deeper into how this powerful medication works and who should consider using it.
E.g. :8 Weeks to Better Metabolism: How Exercise Fixes Insulin Resistance Fast
- 1、How Paxlovid and Other Antivirals Help Fight COVID-19
- 2、The Race Against COVID Mutations
- 3、Important Things to Know Before Taking Paxlovid
- 4、The Future of COVID Treatment
- 5、Beyond Paxlovid: Exploring Other Treatment Options
- 6、The Psychological Side of COVID Treatment
- 7、The Economics of Antiviral Treatments
- 8、Practical Tips for Navigating Treatment
- 9、FAQs
The Power of Early Treatment
Let me tell you something exciting - Paxlovid isn't just for severe cases. This antiviral superstar can help even when your COVID symptoms feel mild. Imagine catching COVID and having a secret weapon that could slash your hospitalization risk by 80%! That's exactly what recent studies show.
Here's the deal: when you take Paxlovid within those crucial first 5 days of symptoms, it's like putting up a force field against serious illness. A massive study tracking over 18,000 people found Paxlovid users were:
| Outcome | With Paxlovid | Without Paxlovid |
|---|---|---|
| Hospitalization Rate | 5% | 25% |
| Death Rate | 1% | 10% |
Who Can Get Paxlovid Right Now?
Currently in the U.S., you'll need to meet certain high-risk criteria to get Paxlovid. We're talking about folks with conditions like diabetes, heart disease, or weakened immune systems. But here's the kicker - researchers are saying we should consider making it available to everyone.
Why? Because Canadian researchers crunched numbers from 41 different trials and found something amazing. For every 1,000 COVID cases, Paxlovid prevented 46 hospitalizations. Even molnupiravir, another antiviral, prevented 16 hospitalizations per 1,000 cases.
The Race Against COVID Mutations
 Photos provided by pixabay
Photos provided by pixabay
Why Variants Keep Scientists on Their Toes
Ever wonder why we can't just declare victory over COVID? Here's the thing - this virus changes its outfit faster than a teenager before prom! What worked against Delta might not work as well against Omicron's latest spin-off.
Dr. David Cutler puts it perfectly: "Meta-analysis helps when we can't study thousands of patients for years, but we've got to take the results with a grain of salt." Translation? The virus moves fast, and science has to move faster.
The Vaccine vs. Antiviral Debate
Now here's a question that might surprise you: Is Paxlovid actually less effective than your vaccine? Some studies say yes - that for vaccinated folks, the shot alone might protect you just as well as Paxlovid. But before you cancel your Paxlovid prescription, remember this:
The real magic happens when vaccines and antivirals work together. Think of it like wearing both a seatbelt and having airbags - double protection is always better!
Important Things to Know Before Taking Paxlovid
The Medication Mix-Up Danger
Paxlovid doesn't play nice with everyone. I'm talking serious drug interactions that could turn your medicine cabinet into a danger zone. From heart medications to even some herbal supplements, you'll need your doctor to play matchmaker.
Dr. Cutler warns: "We've got to check everything - prescriptions, vitamins, even that turmeric supplement your yoga instructor recommended." It's not that Paxlovid is bad - it's just very particular about who it hangs out with.
 Photos provided by pixabay
Photos provided by pixabay
Why Variants Keep Scientists on Their Toes
Here's another head-scratcher: Why does timing matter so much with antivirals? The answer's simple - these drugs work best when they catch the virus early, like stopping a snowball before it becomes an avalanche.
Dr. Johannes nails it: "We need people testing at the first sniffle, not waiting until they can't breathe." That's why having COVID tests ready at home could be a game-changer for getting treatment fast.
The Future of COVID Treatment
Living With COVID - The New Normal
Let's be real - COVID isn't going away. But here's the good news: with tools like Paxlovid, we're learning to live with it. Johannes puts it perfectly: "These treatments won't eliminate COVID, but they'll help keep people out of hospitals and save lives."
Think about how we handle the flu - we've got Tamiflu for bad cases, but mostly we manage. That's where we're heading with COVID, just with better science backing us up.
What This Means for You
If you're high-risk, have that conversation with your doctor now - don't wait until you're sick. Know your options, understand the risks, and make a plan. Because here's the truth: knowledge is the best antiviral we've got.
And remember - while Paxlovid is great, it's not a replacement for vaccines, masks, or common sense. It's another tool in our toolbox, and the more tools we have, the better we can protect ourselves and each other.
Beyond Paxlovid: Exploring Other Treatment Options
 Photos provided by pixabay
Photos provided by pixabay
Why Variants Keep Scientists on Their Toes
You know what's wild? While everyone's talking about Paxlovid, we've got these secret weapons called monoclonal antibodies that don't get enough attention. Picture this - lab-made proteins that mimic your immune system's ability to fight off viruses. They're like giving your body a temporary superhero squad!
Here's something fascinating I learned from Dr. Sarah Thompson at Johns Hopkins: "When Omicron first hit, we had to scramble to develop new monoclonal antibodies because the old ones stopped working. That's how fast this virus changes!" The cool part? These treatments can help people who can't take Paxlovid due to drug interactions.
Natural Remedies That Actually Help
Now don't get me wrong - I'm not saying you should ditch medical treatment for essential oils. But did you know certain natural approaches have real science backing them up? Take zinc for example - studies show it can shorten cold symptoms by about 2 days when taken early.
Vitamin D is another big one. A massive UK study found people with low vitamin D levels were more likely to test positive for COVID. But here's the kicker - you can't just megadose when you get sick. Dr. Thompson told me: "It's like building a strong foundation - you want good vitamin D levels before infection hits."
The Psychological Side of COVID Treatment
How Fear Affects Treatment Decisions
Let's talk about something we don't discuss enough - the mind games COVID plays on us. Have you ever noticed how some people refuse treatment because "it's just a cold," while others demand Paxlovid for a sniffle? There's actually a name for this - it's called the dual reality phenomenon in pandemic psychology.
Dr. James Peterson, a behavioral scientist, explained it to me this way: "We've got two extremes - the minimizers who underestimate risk, and the catastrophizers who overestimate. The sweet spot is in the middle where we take reasonable precautions without panicking."
The Placebo Effect in COVID Recovery
Here's a mind-blowing thought - could some of Paxlovid's benefits actually come from the placebo effect? Before you think I've lost it, hear me out. A recent study found that simply believing you're receiving effective treatment can reduce symptom severity by up to 30%!
But here's the important distinction - this doesn't mean the drug doesn't work. It means our minds and bodies work together in healing. As Dr. Peterson puts it: "The best outcomes happen when we combine effective medicine with positive expectation." That's why bedside manner matters so much in COVID treatment.
Why These Drugs Cost What They Do
Let's get real for a second - have you seen the price tag on some of these treatments? A single dose of certain monoclonal antibodies can cost thousands! But here's what most people don't realize - developing these drugs is insanely expensive.
Check out this comparison of development costs:
| Drug Type | Average Development Cost | Time to Market |
|---|---|---|
| Traditional Antiviral | $1-2 billion | 10-15 years |
| COVID Antiviral | $500 million-$1 billion | 1-2 years |
| Monoclonal Antibody | $200-500 million | 6-18 months |
Insurance Coverage Headaches
Here's where things get messy - insurance coverage for these treatments is all over the map. Some plans cover Paxlovid completely, others make you jump through hoops. I talked to Mark Johnson, an insurance expert, who said: "We're seeing massive variation between states and even between different plans in the same state."
The good news? Many manufacturers have patient assistance programs that can help cover costs if your insurance falls short. The bad news? You often have to do the legwork to find these programs yourself.
Building Your COVID Action Plan
Let me share something personal - I keep what I call a "COVID go-bag" ready at home. It's got rapid tests, a thermometer, pulse oximeter, and a list of medications I'm on. Why? Because when you're sick with a 102° fever, you don't want to be scrambling to remember your medical history!
Here's a pro tip from my doctor: "Have a conversation with your healthcare provider now about what treatments you'd qualify for if you got COVID. Don't wait until you're sick and can't think straight." Smart, right?
When to Push for Treatment
This one's important - know when to advocate for yourself. If you're high-risk and testing positive, don't take "wait and see" for an answer. A nurse friend told me: "We're seeing too many patients who waited too long to seek treatment because they didn't want to 'bother' anyone."
Remember - early treatment makes all the difference. As my grandma used to say: "Better to be the healthy person at the doctor's office than the sick person in the ER!"
E.g. :What doctors wish patients knew about COVID-19 oral antivirals ...
FAQs
Q: How effective is Paxlovid against COVID-19?
A: Let me break it down for you - Paxlovid is incredibly effective when taken early. The latest research shows it reduces hospitalization risk by 80% and death risk by 90% compared to no treatment. That's not just good - that's potentially life-saving! We're talking about real numbers here: for every 1,000 people treated, about 46 hospitalizations are prevented. The key is taking it within those first 5 days of symptoms, when the virus is still getting established in your system. Think of it like stopping a snowball before it becomes an avalanche.
Q: Who can currently get Paxlovid in the United States?
A: Right now, the U.S. limits Paxlovid to people at higher risk for severe COVID-19. This includes folks with conditions like diabetes, heart disease, obesity, or weakened immune systems. But here's what's interesting - Canadian researchers found that expanding access could benefit everyone. I've talked to doctors who say the current restrictions might be too tight, especially since the medication works so well when given early. If you're unsure whether you qualify, your best bet is to check with your healthcare provider about your specific risk factors.
Q: How does Paxlovid compare to COVID-19 vaccines?
A: This is a great question! Vaccines and Paxlovid work differently but complement each other perfectly. While vaccines teach your immune system to recognize COVID-19 beforehand, Paxlovid jumps into action if you do get infected. Some studies suggest vaccines alone might protect as well as Paxlovid in vaccinated individuals, but here's how I see it: why not use both? It's like wearing a seatbelt and having airbags - double protection is always better when it comes to your health.
Q: What are the risks or side effects of taking Paxlovid?
A: The main concern isn't so much side effects as drug interactions. Paxlovid doesn't play nice with many common medications, including some heart drugs, blood thinners, and even herbal supplements. That's why your doctor will need to review everything you're taking before prescribing it. The good news? Most people tolerate Paxlovid well when it's used appropriately. Just remember - this isn't something you should take "just in case." It's a powerful medication that needs proper medical supervision.
Q: Should I wait for severe symptoms before taking Paxlovid?
A: Absolutely not! In fact, that's one of the biggest mistakes people make. Paxlovid works best early in the infection, typically within 5 days of symptom onset. Waiting until you're severely ill means you've missed the window when the medication can do its best work. That's why testing at the first sign of symptoms is so crucial. As Dr. Johannes told me, "We need people testing at the first sniffle, not waiting until they can't breathe." Don't hesitate - early action could make all the difference.